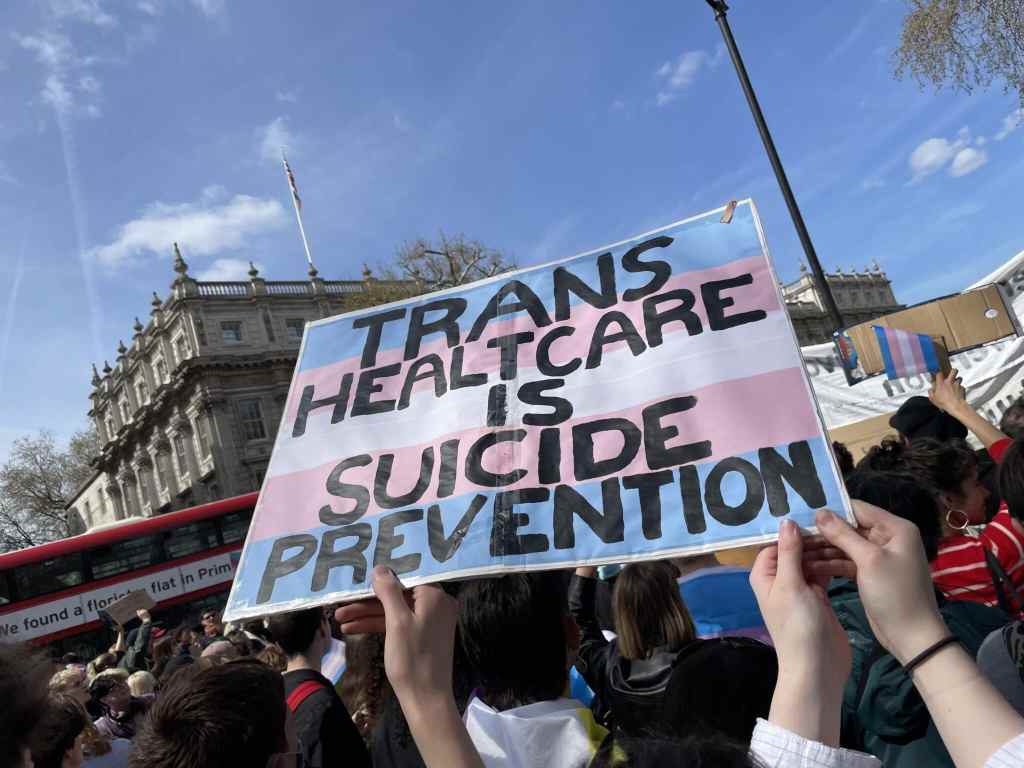
New independent surgical guidelines created to ‘ensure the safety and dignity of trans patients’

A new set of guidelines, produced independently of the NHS, have been created for trans surgical patients (Canva)
A new set of guidelines, produced independently of the NHS, have been created for trans surgical patients (Canva)
A new set of guidelines, independent of the NHS, have been created for trans surgical patients, with the aim of guiding “best practice to ensure the safety and dignity of transgender and gender-diverse people in the peri-operative period”.
The peri-operative period lasts from the moment the patient goes into the hospital until they go home.
The guidance notes that trans people “face significant health inequity and that healthcare professional knowledge, and practice specific to their care, must improve.”
Published in Anaesthesia, the journal of the Association of Anaesthetists, the guidance is described by its authors as a first-of-its-kind to look specifically at peri-operative considerations, and sets out 15 recommendations for the care of trans men and women, including the use of preferred name and pronouns and caring for them in an environment that respects their gender identity.
“While transgender and gender-diverse people may have specific health needs in relation to gender dysphoria, their health requirements go beyond their gender identity,” the introduction reads.
“Most doctors will provide care to someone who is transgender or gender-diverse at some stage in their career. It is, therefore, important that all anaesthetists are educated on specific considerations when caring for these patients.”
To create the guidance, a working group of individuals with experience in direct clinical care of trans people, including “those who have expertise in endocrinology and gender-affirming hormones, educators on the topic of transgender and gender-diverse healthcare, and authors of both cisgender and transgender identities”, were brought together to discuss and review literature on the topic.
The authors initially came up with a list of more than 25 recommendations but these whittled down to 15, following further review by the working party.
The first recommendation focuses on the use of a patient’s name and pronouns as an “important way of showing respect and decreasing the risk of gender dysphoria” while another calls for a “process whereby a patient can privately and safely disclose both their sex at birth and gender, as part of pre-operative assessment”, adding that digital pre-assessment questionnaires can provide this “in an elective setting”.
Another recommendation asserts hormone therapy should be continued throughout the peri-operative period “unless there are specific contraindications”, and “patients should be counselled on the risks and benefits of this, with the aim of making a shared decision”.
The guidance also says members of the transgender community should be cared for in an environment that “respects their gender identity”, which “in some circumstances, may involve providing a single room”.
Speaking to the BBC, co-author Dr Stuart Edwardson said: “It is significant because we know there is a dearth of knowledge and confidence among anaesthetists when caring for transgender and gender-diverse patients.
“Importantly, [the guidance] seeks not to answer any of the legal or societal questions surrounding transgender people at the moment, but instead… to make sure their every-day healthcare is as safe and dignified as it can be.”

